When Associate Professor Myriam Heiman began studying neuroscience as a postdoc, scientists interested in neurodegenerative diseases had long reported evidence of inflammation, or the activation of immune responses, but few were claiming it was an early driver of disease.
“It was initially thought it might be perhaps more of a secondary response to neural damage,” Heiman said.
Similarly, in the late 1990s as Picower Professor Li-Huei Tsai began focusing her research on understanding Alzheimer’s disease, she had no inkling of how deeply she would now be delving into the central nervous system’s immune activity.
But over the last several years research has increasingly shown that immune activity may have a core role in the progression of neurodegenerative diseases. Even when researchers don’t set out in search of immune impacts, they find them anyway. Using broad, unbiased methods to detect ways in which cellular and molecular activity is altered by disease, Tsai and Heiman have each recently discovered specific new ways in which immune activity appears to be more prominent and consequential in Alzheimer’s and Huntington’s disease respectively.
Above: A cartoon depicts microglia, the brain's immune cells (green), amid globs of the Alzheimer's disease hallmark amyloid protein (yellow) and inflamed neurons (red). Image by Sputnik Animation.
“Our recent studies indicate it might be more of an initial contributor to pathogenesis," Heiman said. “There’s a theme emerging across the studies of our labs and others in the community that perhaps neural inflammation isn’t just a secondary reaction, but maybe among the primary toxicity mechanisms as well.”
Tsai agrees: “Neural inflammation is a defining feature of Alzheimer’s disease.”
“The important thing to keep in mind is that these are new hypotheses in fields that have been wanting for therapeutics for decades,” Heiman said. “It could be that there are immune relevant pathways that were underappreciated.”
And while neuroscientists once insisted that the brain was “immune privileged,” which is to say they thought it did not interact with the rest of the body’s immune system, Mark Hyman Jr. Associate Professor Gloria Choi is among a small community of neuroscientists who are finding exactly such connections between peripheral immune system activity and the brain, including a link between maternal infection and the development of autism-like social deficits in offspring. By dedicating her lab to the study of how the immune and central nervous systems interact to influence brain function, disorders and social behavior, Choi has joined the vanguard of a relatively new field: “neuroimmunology.”
Activity in Alzheimer’s
In a recent review paper co-authored with graduate student Mitch Murdock, Tsai analyzed a recent outpouring of evidence neuroscientists have produced about Alzheimer’s using “single-cell” techniques, in which they can assess how cellular activities such as gene expression differ in healthy brains vs. ones afflicted with disease. Tsai and Murdock found that in each of five major brain cell types, including neurons, one of the five most prominent changes were increases in immune and inflammatory activity. Moreover, Tsai says, other studies are showing that expression of genes associated with increased Alzheimer’s risk, including the one of the most common, APOE4, is pronounced in many immune cells.
Tsai’s own research employing broad-based single-cell sequencing techniques to better understand Alzheimer’s has been revealing the importance of immune activity in the brain for years. In 2015 her lab collaborated with that of MIT computer scientist Manolis Kellis to show that the brains of Alzheimer’s patients and lab mice modeling the disease both developed heightened genetic predisposition to inflammatory activity, particularly because of the enhancement of a gene transcription factor called PU.1 (now seen as a promising therapeutic target).
“We showed that the immune response is an extremely early event way before neurodegeneration,” Tsai said.
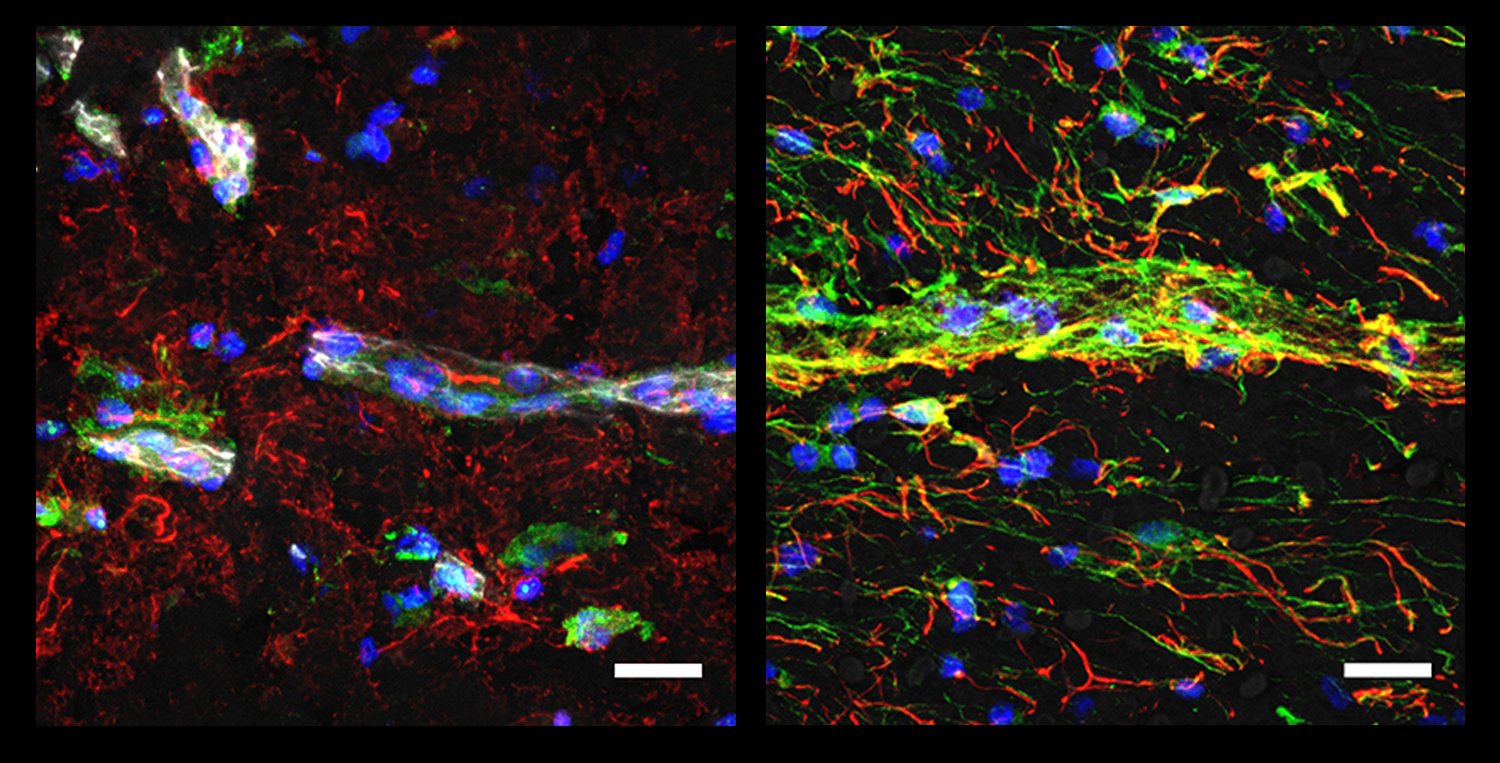
Indeed in 2017 the lab followed up with a study focusing on how gene expression changed in the brain’s resident immune cells, called microglia, as disease progressed. They found evidence that some microglia change their activity early and dramatically in disease, potentially triggering a cascade of inflammation that leads to neuron death.
And two studies published by Tsai’s lab in just this past year illustrate new complexities of immune activity’s integral role in Alzheimer’s disease.
Postdoc Matheus Victor led a study published in August in which the lab sought to understand how APOE4 affects microglia. The APOE gene, of which APOE4 is a harmful variation, determines how cells handle fat molecules called lipids. APOE4 microglia, they found, are prone to becoming inflammatory, rendering them less adept at processing lipids. They accumulate more of the molecules, clear away less, and that, in turn, impedes the ability of nearby neurons to communicate by disrupting the potassium ion receptors they use to regulate electric charge.
Just a month later, graduate student Gwyneth Welch led the Tsai lab’s discovery of another problematic immune interaction between neurons and microglia. When encoding memories, neurons normally snap open their DNA for quick gene expression, Tsai’s lab has found that over time and with age, these breaks aren’t repaired as well as they should be and therefore accumulate. Welch found that when this happens neurons emit molecular immune activation signals as if calling to microglia for help, a phenomenon that had not been observed before in Alzheimer’s disease. The microglia respond to this neural instigation, but in an inflammatory way that leads to a degradation of neural circuit connections called synapses.
It’s not clear why immune responses, which are surely meant to protect health, can instead come to undermine it, but Tsai notes that the classic immune role of fighting off a pathogen is meant to be a short-term battle. In cases such as the double-stranded breaks associated with neurodegeneration, the problem is problematically prolonged.
“A pathogen invasion is an acute event,” Tsai said. “The pathogen’s there, microglia come in, get rid of whatever, and it’s over. But I think the DNA breaks are pervasive. It's a chronic condition. So that that leads to a cascade of events and it almost becomes the immune system attacking the self.”
Happening in Huntington’s
In her Huntington’s disease research, Heiman has found evidence of what appears to be self-inflicted neuron death. In a 2020 study led by postdoc Hyeseung Lee, she teamed up with Kellis to assess gene transcription and translation in Huntington’s disease patients and in model mice in neurons that have proven to be especially vulnerable in the disease. To their surprise they saw RNA not only from the nucleus, but also leaking from cells’ damaged mitochondria. They also saw evidence of a highly elevated immune response to this misplaced genetic material that, to the cell, might have looked foreign. The inwardly turned immune response, signaled at least in part by the protein PKR, is likely toxic to the cell although the lab is following up to determine if it’s really causal, Heiman said. But what’s remarkable already, she said, is that this was the neuron’s own “innate” immune response to its own mitochondrial RNA, which had not been appreciated before.
“What was surprising was how early we saw this innate immune activation in neurons in Huntington’s disease,” Heiman said.
In a 2022 study led by graduate student Francisco Garcia that mapped cell types in the brain’s vasculature, Heiman and Kellis’s labs found that in Huntington’s disease PKR was also elevated in the endothelial cells that constitute the brain’s blood vessels. The increased immune activity was strongly correlated with a loss of proteins that help form the blood-brain barrier, which could interfere with the brain’s ability to keep out harmful substances.
Heiman hypothesizes that knocking down expression of PKR in cells might tamp down these potentially toxic immune responses.
Heiman’s lab has also found other indications of immune response problems in Huntington’s disease. In another study in 2020 led by postdoc Mary Wertz, her lab became the first to perform a genome-wide screen in mice of the consequences of knocking out each of 22,000 genes in neurons to see which genes, when lacking, proved lethal compared to leaving it alone in unaltered controls. The screen therefore revealed which genes were essential for neuronal survival. The lab then also did the screen in mice modeling Huntington’s disease so that they could see, by comparison, whether knocking each gene hurt neurons or helped. Among the “hits” in that work was the gene for a signal transducer for the immune signaling molecule Interleukin-6 (IL-6) among other molecules. Knocking it out seemed to benefit neural survival in Huntington’s disease.
That result seemed to square with clinical reports suggesting that Huntington’s disease patients experience elevated levels of IL-6 years before they show clinical symptom onset. Researchers including Heiman hypothesized that knocking out or blocking IL-6 receptors would therefore make Huntington’s disease model mice healthier, but in a study later that year led by Wertz the lab surprisingly showed the opposite. Digging deeper into gene expression differences made by having IL-6 vs. not having it, Heiman’s lab noted that in a normal (non diseased) context the molecule may promote healthier synaptic connections among neurons. It may be that normal levels of IL-6 aren’t the problem but that higher levels in disease are. Unresolved thought it may be, the finding is still a lead that could yield a therapeutic target.
“The important thing to keep in mind is that these are new hypotheses in fields that have been wanting for therapeutics for decades,” Heiman said. “It could be that there are immune relevant pathways that were underappreciated.”
Bearing on behavior
Choi’s work, meanwhile, is showing that immune pathways from beyond the brain (and maybe from the brain back out to the body) have profound impacts on brain functions, especially including social behavior.
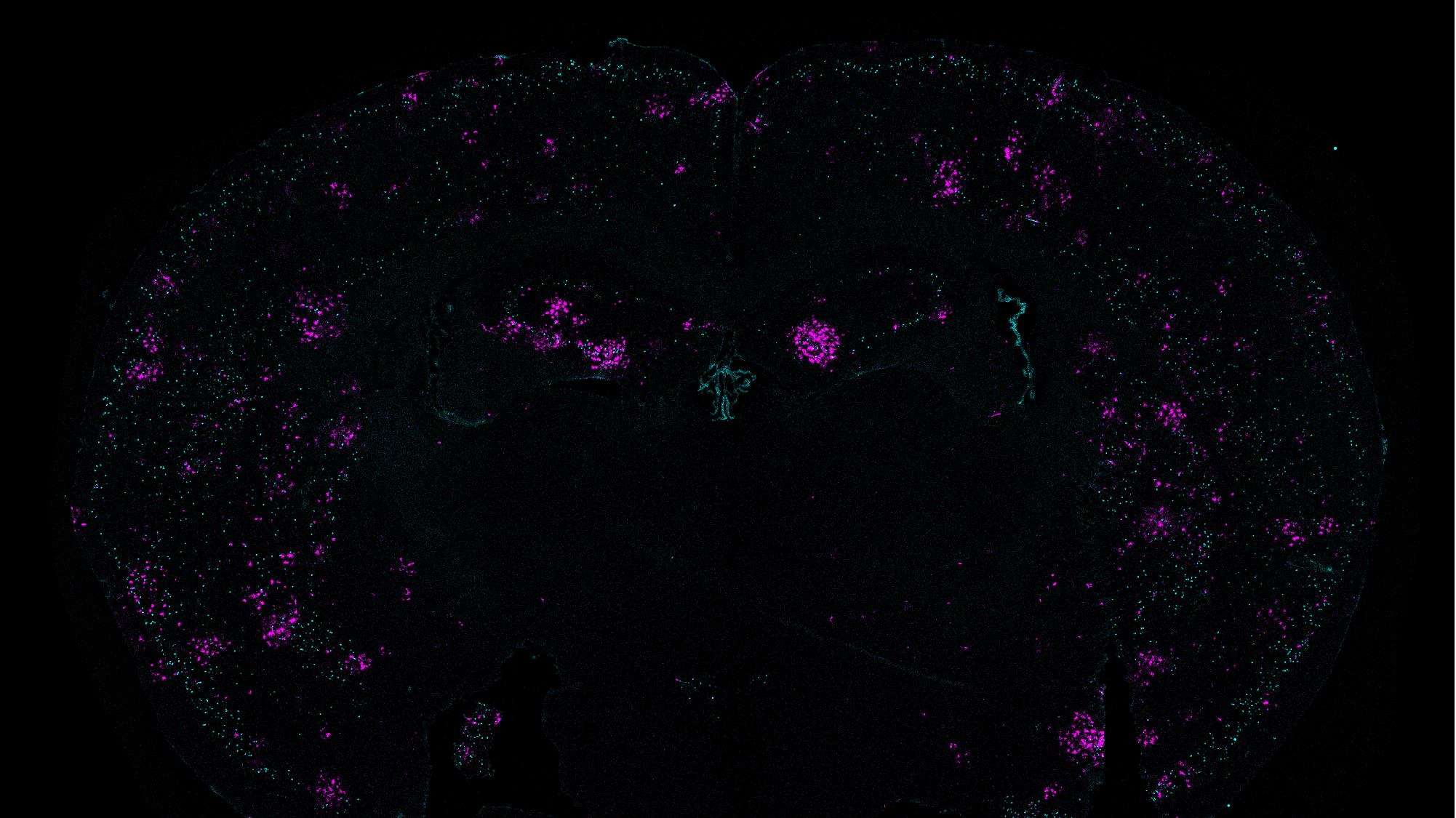
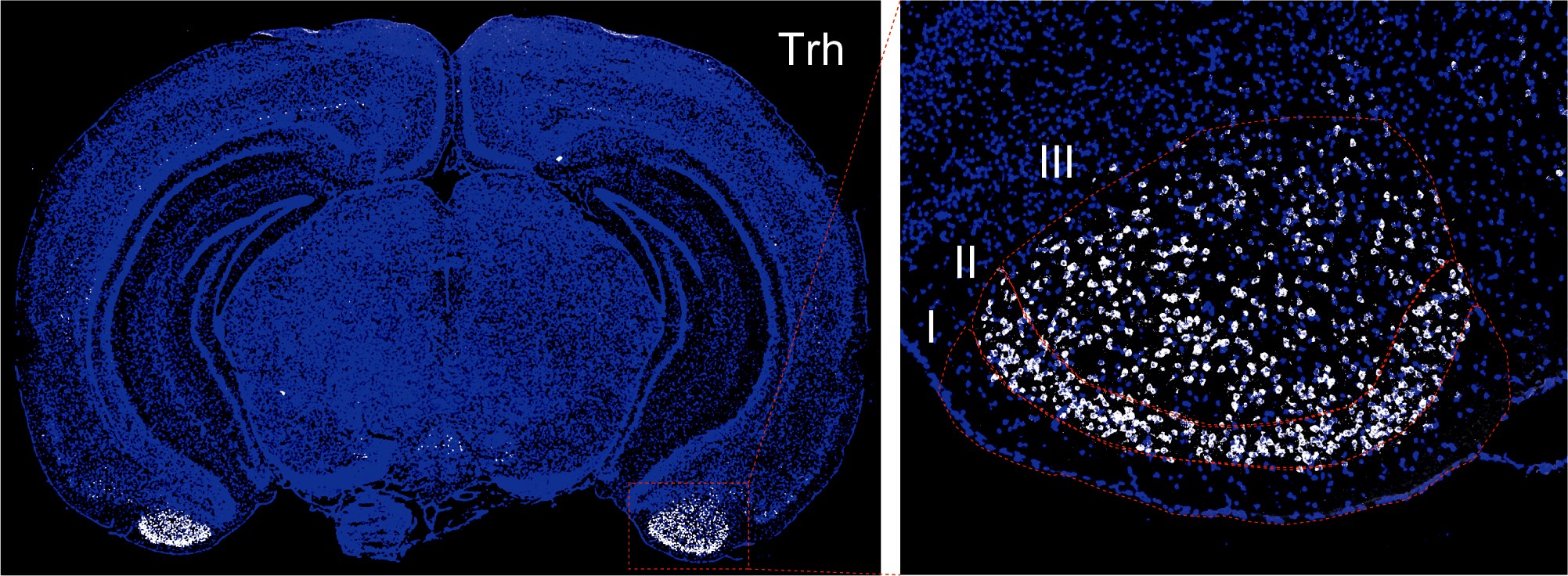
Choi launched into neuroimmunology field not long after starting her MIT lab in 2013. She and her husband Jun Huh, an immunology associate professor at Harvard Medical School, decided to tackle a puzzling clinical question: Why is infection during pregnancy associated with the development of autism in the child? Over several years the couple’s labs found the link in mouse models: When a pregnant mouse has certain bacteria in her microbiome and becomes infected, immune cells overproduce the cytokine IL-17a. The molecule reaches receptors in the fetal brain. Cortical development in the fetus becomes disrupted and is characterized later in life by neural hyperactivity in circuits leading from the S1DZ region of the cortex to areas affecting social behavior, producing autism-like symptoms. Choi is now looking more deeply at IL-17a’s role in the S1DZ region, as well as its links to social behavior.
In 2021 Choi’s lab also found a specific brain circuit that enforces a form of social distancing. Led by postdoc Jeongtae Kwon, the lab showed that when a male mouse smells that a potential mate is ill, he will restrain that mating instinct. Published amid peaks of Covid-19 surges, the study provided a timely link between social behavior and immune behavior that the lab is continuing to study intently. In early-stage experiments the lab is finding that some degree of social interaction (but not mating) between apparently sick and well cage mates “primes” the immune system of well mice such that when they are then challenged with infection they fare better than cage mates who don’t have any interaction with a sick cage mate. Relatedly, postdoc Yire Jeong recently earned a competitive grant from the MIT School of Science John W. Jarve (1978) Seed Fund for Science Innovation, to investigate why group-housed mice appear to fight off sickness better than isolated mice upon exposure. Jeong’s hypothesis, Choi said, is that social interaction may affect immune pathways from the brain to perhaps prime immune cells.
“There's a benefit to social interaction, but also there's a risk that comes from interacting with the others in terms of increased exposure to infections,” Choi said. “Many of the interactions between the immune system and brain may have evolved to modulate social behaviors because social behaviors, I think have such a profound impact on how we deal with pathogens.”
Choi is also embarking on new studies to systematically survey the brain for other receptors for immune system molecules—cytokines and chemokines—like the ones that give IL-17a a foothold in the brain. With funding from MIT’s Aging Brain Initiative and the Ludwig Family Foundation, she’s also looking at how this changes with age.
“One of the major things we're trying to do is to map out all the communication channels through which the immune system can influence brain function,” Choi said. “By doing that we've been discovering how different cytokines and chemokines can modulate different brain regions in neural circuits for specific behaviors or internal states.”
For instance, early data indicates that immune system molecules in the brain can affect anxiety and feeding behaviors, Choi said.
Such studies by Choi, Tsai and Heiman are all among the forefront of a transition in neuroscience in which the field has been moving from dismissing or merely noting immune activity in the brain to exploring, appreciating and understanding its considerable depth and importance in health and behavior.