Keeping an eye open for change
Ip and co-authors employed the time-honored protocol of “monocular deprivation,” or temporarily shutting one eye for a week. Normally, responses in visual cortex neurons related to the closed eye become weaker, but responses related to the remaining open eye become stronger, as if to compensate for the change in ability. This neural circuit adjustment to experience is called “homeostatic plasticity.”
In the normal mice, closing an eye for a week had the expected effect. But in mice with one copy of MVP missing, the researchers observed a telling difference. Responses related to the closed eye still weakened, but responses from the open eye did not get stronger. Homeostatic plasticity was disrupted.
“After seeing that MVP is responsible, we asked how MVP does it,” Ip said.
In those further tests, the team found that neurons in MVP-reduced mice experienced less electrical current across their excitatory synapse connections with other neurons, suggesting reduced functional excitatory synapses. They found other differences, too. MVP-reduced mice overexpressed the gene STAT1, an immune-system gene known to be regulated by MVP.
In 2014 Sur’s lab had found that mice without STAT1 have unusually strong open-eye responses after monocular deprivation. Now in the new study, with less MVP than usual and too much STAT1, mice experienced the opposite. Sure enough, when the researchers knocked down STAT1 as well as MVP, they were able to bring back a near-normal open-eye response to monocular deprivation, suggesting that loss of MVP disrupts homeostatic plasticity by allowing for an overabundance of STAT1.
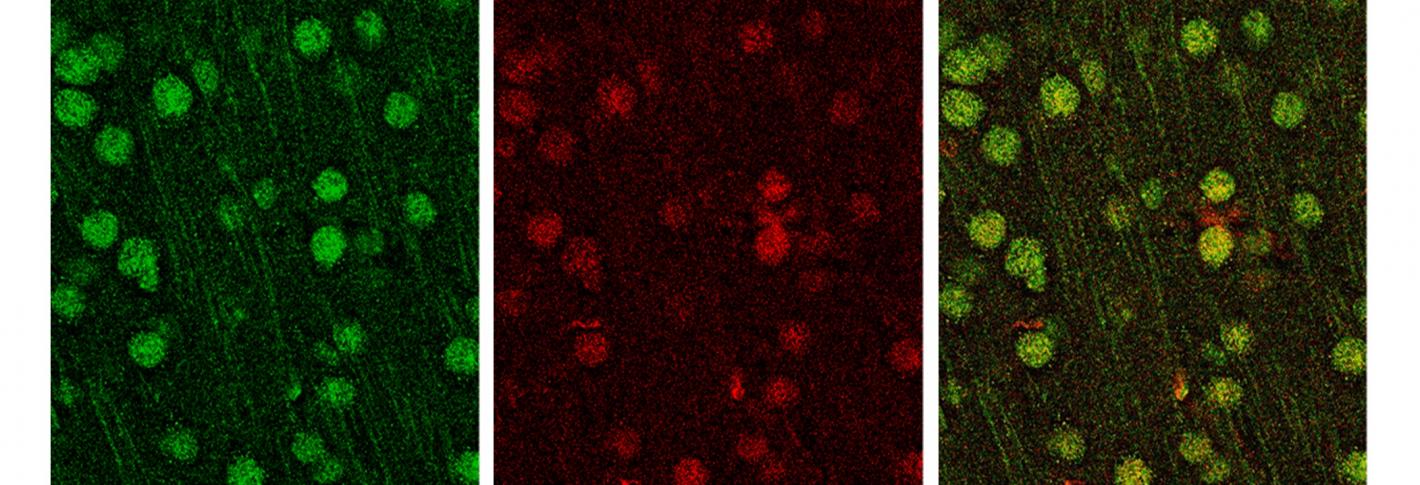
Then Ip, Sur and co-authors dug even deeper. They found that in MVP-reduced mice, neurons weren’t producing the expected open-eye responses because they weren’t expressing a key receptor, the GluA1 AMPA receptor, on the surface of dendritic spines.
Even though the findings were made, by design, in the visual cortex, the authors said they expect the disruption of homeostatic plasticity to occur elsewhere as well.
"This gene's presence is reduced everywhere in the brain," Sur noted.
Relationship with immune system
In addition to illustrating how a specific gene may contribute to the symptoms of 16p11.2 deletion syndrome, Sur said, the findings also raise an intriguing, broader question about the central nervous system: Is it perhaps not a coincidence that some of its ability to adjust to and incorporate experience comes from genes that are also active in the immune system?
“The immune system is really a system of learning and memory,” Sur said. “You get infected and the body makes antibodies and the next time there is a ‘memory’ of the infection. It is conceptually a very similar idea.”
In addition to Ip and Sur, the paper’s other authors are Ikue Nagakura, Jeremy Petravicz, Keji Li, and Erik Wiemer.
The Human Frontier Science Program, The National Institutes of Health (grants: MH085802 and EY007023), and the Simons Foundation supported the research.